News & Insights
News & Insights
BY BPD
The Summit Series is increasingly becoming the forum where industry leaders drop by to share wisdom and learnings about the turmoil and turbulence that have become the norm for health system operators.
That’s what happened when Clint Hailey, SVP & Chief Managed Care Officer of Tenet Healthcare, joined Sasha Boghosian, Chief Strategy & Innovation Officer at BPD, for some straight talk about the challenges facing health systems in today’s healthcare landscape.
Mr. Hailey covered a variety of issues during the hourlong conversation, ranging from what he’s seeing among payors related to prior authorization, to the latest in Medicare Advantage (MA) contracting, and top-of-funnel growth strategy among health systems trying to resolve friction around access barriers for their patients. The audience of nearly a hundred attendees — all health system leaders and industry insiders — engaged with a barrage of questions and comments that made the session feel like an intimate conversation.
During the session, Mr. Hailey also shared his thoughts on capitation, a payment model that has been held up by some as a major lever for addressing rising healthcare costs at scale. In Mr. Hailey’s view, a simple math equation can show the model’s limitations and temper the faith that many in our industry are placing in it.
The view that Mr. Hailey outlined (in just a few minutes, no less) was the simplest and most insightful analysis of capitation we have heard from an industry insider, so we thought it deserved additional airtime.
The promise (and limitations) of capitation
The predominant belief for the last decade has been that the answer to “fixing” healthcare lies in value-based care. More specifically, many experts have put their faith in adopting the Accountable Care Organization (ACO) model and in restructuring the payment model.
In some instances, we’ve seen providers develop payor arms to achieve a degree of vertical integration (you may have heard of the term “payvider”). Others have leaned heavily into capitation, or a predictable, upfront, set amount of money to cover the predicted cost of all or some of the healthcare services for a specific patient over a certain period of time.
But for all its promise, capitation can’t achieve the scale necessary to meaningfully impact healthcare costs. To understand why, you just need to do some math:
333 million. That’s the total US population, so that’s the universe we’re working from.
Now, let’s start subtracting the parts that we can’t capitation...
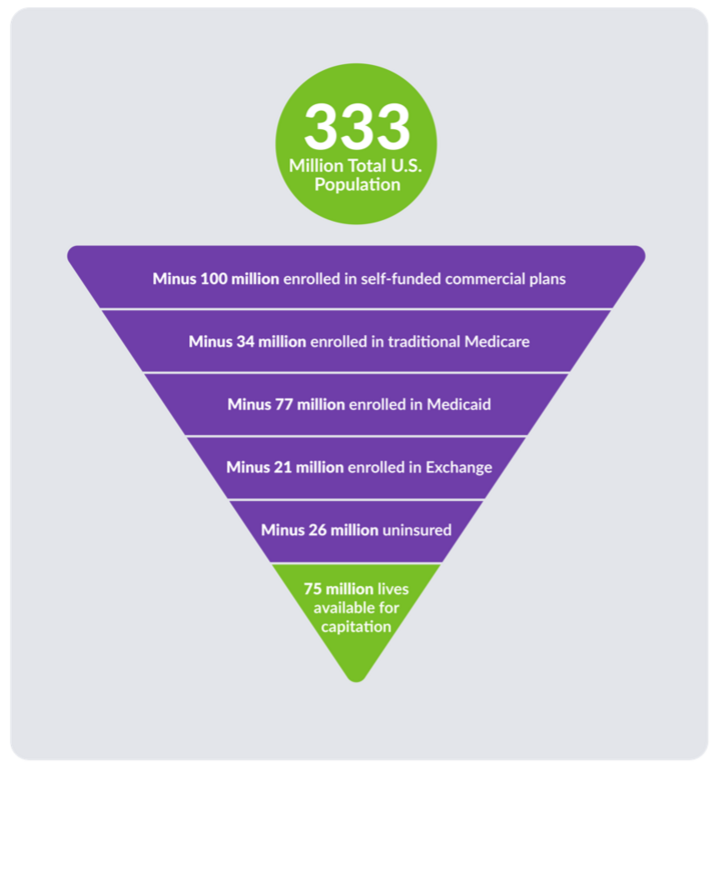
The math above is simple. It’s not possible to capitate the uninsured, self-funded lives, or those covered by exchange plans. This leaves roughly 75 million individuals covered by either fully insured or MA plans that could potentially benefit from capitation. That is simply not large enough to create meaningful impact — or to serve as a universal answer to the complex problem of the cost of healthcare in the United States.
What we can do
“Value-based care” is a term in our healthcare landscape that is used so loosely that it has seemingly lost its core meaning. To reclaim it, we have to go back to the very idea of value and think about it in a different way. The focus needs to shift from overhauling payment models to redefining “value,” including looking beyond conventional metrics like capitation.
Consider the value-story that your organization has, what payors are looking for, and how you can think creatively to find common ground. Instead of a single fix-all, a sustainable path forward likely includes a number of smaller-scale solutions combined. Collaboration with payers, particularly in exploring MA payment reform, is one such opportunity. In fact, if some kind of payment system reform is in our industry’s future, it’s likely going to be limited mainly to the MA space.
Another opportunity is for contracts to evolve into static, stable agreements, with built-in provisions for significant changes, ensuring fairness and sustainability. For example, consider a static contract with a payor for a short period of time, one that limits the amount of ebbing and flowing around reimbursement so there’s recourse when the payor attempts to deviate from the original intent of the contract.
The underlying takeaway is this: there is no single solution that will fix all the turbulence facing health systems or the continued rise in healthcare costs. We must look for innovative approaches, both small and large, that create mutually beneficial value for the payor, the provider, and the patient and don’t rely on unrealistic, miraculous shifts to save the day.
Frank conversations about the challenges we collectively face as healthcare providers — like the ones that BPD’s Summit Series facilitates — are more important than ever if we hope to improve healthcare in meaningful ways.
Related Blog Posts
Stay in Touch
Stay in Touch
Receive our updates, industry news and insights.


